If you’re a teenager who’s excellent at hearing the shimmer of cymbals but struggles with deeper voices—or you’re finding a teacher “just isn’t loud enough” when everyone else seems fine—you’re not imagining things, and you’re not alone. Teen hearing is usually excellent, but two realities can make school and social life harder than they need to be: (1) subtle hearing changes that don’t show up on a basic “free check,” and (2) Auditory Processing Disorder (APD), where the ears hear b”t the brain”works harder to make sense of sound—especially in noise. Sometimes both are in the mix. A thorough diagnostic hearing assessment can quickly untangle this and provide you with practical steps to feel more in control in the classroom, with friends, and at home.
Why a proper diagnostic test (not just a quick screen) matters
Retail “free hearing tests” are helpful as a first screening tool, but they’re brief and designed to flag apparent hearing loss in adults whomayt need hearing aids. Teen hearing concerns are different. You might notice trouble with low-pitched speech, mumbled voices, or listening when there’s background noise. You might already have an APD diagnosis and assume “ithere’st processing,” but a change in what you hear—like deeper notes in a song dropping out, or ma”e voices feeling softer—warrants a complete diagnostic work-up.
At The Audiology Place, a teenager’s assessment is a 60–90 minute appointment in a quiet, sound-treated room. The assessmentss thoroughevaluation is necessary because subtle issues are easy to, miss on quick screen,s and because the right plan depends on a correct diagnosis.
What we test (and why)
1) Pure-tone audiometry (including low frequencies).
You’ll hear beeps ranging from very low pitches to very high ones. We check each ear carefully and can extend low-frequency testing if you’re noticing bass notes or low voices are harder to catch. Low-frequency hearing changes can be related to middle-ear fluid, Eustachian tube issues, or (more rarely) inner-ear causes. Knowing which one it is is essential.
2) Tympanometry and acoustic reflexes.
This checks how well your eardrum and middle ear move. It helps us spot congestion, pressure problems, or fluid—common reasons teens miss low pitches or describe ears as “full.”
3) Speech understanding in quiet and in noise.
Real life isn’t a quiet booth. We measure how well you understand words and sentences at normal and soft levels, and then repeat them while adding background chatter. If you say,” I hear the teacher but can’t understand them when the room is noisy,” this test shows exactly how big that gap is.
4) OAEs (Otoacoustic Emissions).
These are tiny echoes from the inner ear’s outer hair cells—helpful in detecting early or subtle inner-ear changes even when the standard audiogram looks “normal.”
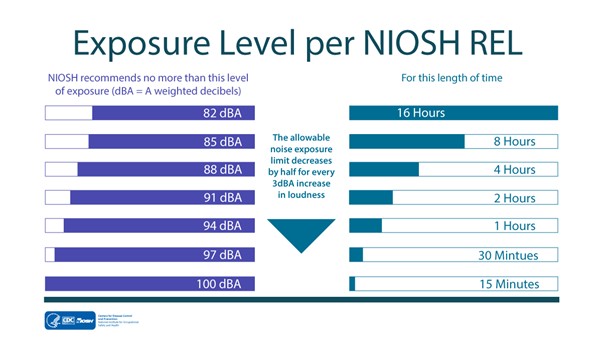
5) High-frequency or extended audiometry (as needed).
If you’re a musician, a frequent headphone user, or spend time in noisy environments, we may check for the highest pitches to detect early signs of change.
6) APD-focused measures (if indicated).
If there’s already a diagnosis of APD—or strong suspicion—we’ll consider targeted tests such as:
LiSN-S (listening in spatialized noise) to assess how you use voice and spatial cues;
Dichotic listening (how each ear handles different information at the same time);
Temporal processing (gaps-in-noise, pitch or duration patterning) to see how you track rapid changes in sound.
These aren’t “pass/fail.” They map how you process sound so we can design practical strategies that work at school.
APD vs hearing loss: how to tell the difference
Hearing loss is primarily about audibility—sounds aren’t reaching the brain clearly or at a normal level of strength. You’ll see this on the audiogram (the graph of your hearing thresholds), and speech often feels soft or muffled.
APD is about efficiency—sounds arrive, but your brain has to work harder to separate the teacher’s voice from the classroom, follow fast instructions, or keep up when the content is dense. Your basic hearing thresholds can be normal, but speech-in-noise and specific processing tests reveal where the bottleneck is.
You can have both. That’s why a full battery—thresholds, middle-ear checks, speech tests, and APD measures—matters. Once we know what’s driving your difficulties, we can tailor support: medical treatment for middle-ear issues, hearing devices if there’s clinically significant loss, or classroom/technology strategies if APD is the main factor.
“Is it worth getting tested if it might be ‘normal’?”
Yes—because “normal” on a quick test doesn’t answer the real-world question: why does listening feel hard? Even if your hearing thresholds are normal, we can still document speech-in-noise challenges, identify processing patterns, and write a school-friendly management plan. That plan can unlock practical supports—like remote microphone systems, innovative seating, captioning, note-sharing, and teacher strategies—so you’re not battling the room every lesson.
If you notice a sudden change in your hearing, ear pain, pressure, dizziness, or a one-sided problem, see your GP promptly and inform them that it’s urgent. Sudden changes should be assessed quickly.
Costs, referrals and who pays for what (Australian context)
A few simple pointers help keep this straightforward and affordable:
Medicare rebates: With a GP referral for diagnostic audiology, you can usually claim a Medicare rebate for tests performed by a Medicare-eligible audiologist. There may still be an out-of-pocket “gap,” which varies by clinic. We’ll explain the fees upfront and provide you with the correct receipt to claim your rebate.
HSP (Hearing Services Program) & Hearing Australia: Young people under 26 may be eligible for services through Hearing Australia’s Community Service Obligations. That pathway can cover diagnostic care and, if clinically indicated, hearing devices with little or no cost for standard options. If you’ve been quoted a fee you don’t understand, ask for it in writing—eligibility and inclusions can be clarified.
NDIS: For hearing supports via the NDIS, you need to meet their access criteria (the impairment must be permanent and significantly impact daily life). There isn’t a single dB “magic number” for everyone; evidence from your assessment, school/uni reports, and functional impact all matter. Many teens with APD but normal hearing thresholds use non-aid supports (remote mics, classroom adjustments, strategy training) rather than hearing aids.
University clinics and public hospitals: If cost is your primary barrier, ask your GP about referring to a public hospital audiology clinic or a university teaching clinic (e.g., Macquarie, Sydney). They often have reduced fees and excellent clinicians.
If you’d like, we can help you navigate these paprovidend provide a written quote bmake a decisionyou make a decision.
What we do with the reYou’ll leavelleave with clear answers and a plan. That might include:
Medical referral if we find a middle-ear problem or anything needing ENT review.
Targeted strategies for APD: seating plans, pre-teaching key terms, captioning, study skills for auditory memory, and teacher tips to reduce the rate of speech and increase clarity.
Technology supports include remote microphone (teacher-worn) systems that stream the teacher’s voice directly to your ears (with or without hearing aids), personal FM systems, or noise-management features on your devices.
Hearing aids or hearables (only if indicated): These are recommended when a clinically meaningful hearing loss is present. Fittings are evidence-based (we use real-ear measures and speech-in-noise validation) and focused on the environments you care about—classrooms, music, gaming chat, or sport.
A school-ready report: Plain-language recommendations your school or uni can implement right away.
Practical signs it’s time to book
You miss deeper voices, bass notes, or say “everyone mumbles,” especially in group settings.
One voice—often a teacher—seems consistently too soft when others don’t notice.
You’re exhausted by listening, grades dip in talk-heavy subjects, or instructions don’t “stick.”
You already have APD, and things have changed, or new symptoms (blocked ears, fullness, tinnitus) have appeared.
Family or friends notice you say”“huh?” more, or you prefer captions even at normal volumes.
A quick word on sales pressure
Teenagers rarely need hearing aids—and never after a ten-minute screen. If anyone rushes you toward a device without a thorough diagnostic assessment and clear explanation, pause. Ask for the clinician’s qualifications (look for Audiology Australia membership) and for your results in writing. You’re entitled to a second opinion.
How The Audiology Place can help
We’re independent—no brand quotas, no one-size-fits-all bundle. Your first full hearing test and consultation takes around 90 minutes in our sound-treated clinic in Forestville (Northern Beaches). Dr Signe Steers has nearly 20 years of experience in paediatric and teen audiology, APD assessments, and evidence-based fittings when needed. We’ll
Listen to your specific concerns (such as low voices, music, or classroom noise).
Run the proper tests the first time—including speech-in-noise and APD measures where appropriate.
Explain every result in plain English.
Map out a step-by-step plan for school, home, and study—devices only if indicated.
Help you navigate GP referrals, Medicare rebates, and, where relevant, HSP/NDIS pathways.
If cost isa concerny,letl usknow when you book—wewe’llutline options (including university clinics or staged care) so you can choosewith confidencey.